As the rate of confirmed cases of the coronavirus neared its firsts peak in the US in March and April 2020, many hospitals nationwide faced a significant shortage of ventilators, leaving many patients in need.
In response to this shortage, many companies and student teams have worked to design and build low-cost ventilators that often work by compressing volumes of air at set frequencies to force air into patients. This type of solution, however, can be problematic. In many COVID-19 patients, acute respiratory distress syndrome (ARDS) impedes alveoli in the lungs from reopening after each breath. Affected parts of the lungs begin to cease functioning normally and eventually collapse (atelectasis). To try to force the remaining parts of the lungs open with a mechanical bag ventilator is not only uncomfortable, but also puts the patient at risk of barotrauma, or tissue damage due to excessive air pressure.
However, medical professionals have been able to help patients maintain healthy blood oxygen levels by treating them with devices providing positive end expiratory pressure (PEEP). In a guidance document released in March, the FDA has suggested the use of alternative devices able to provide PEEP for adapted emergency COVID-19 use, in the event that the country’s supply of ventilators were to run low.
As a team of Berkeley students, faculty, professors, and UCSF/Kaiser physicians lead by Prof. Grace O’Connell, we set out to design and manufacture a simple, low-cost ventilator by outfitting conventional CPAP and BiPAP machines otherwise used for sleep apnea treatment. This device was beneficial for patients in need of moderate breathing assistance or for those weaning off of full ventilation, freeing machines for patients with more severe cases of respiratory difficulty.
Thanks to donations from folks across the San Francisco Bay area, our group received over 1,000 CPAP and BiPAP machines to supply ventilators to high need areas such as New York City and Northern California.
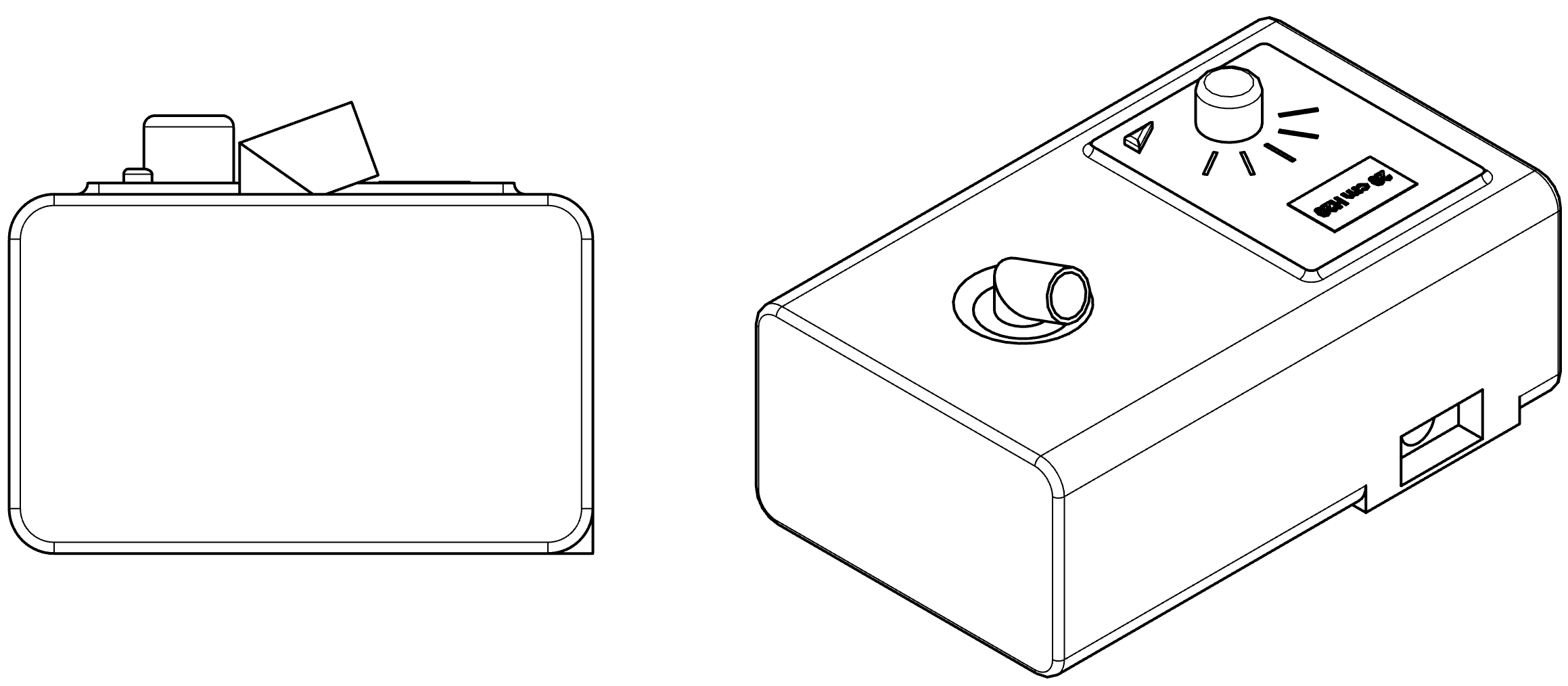
While the sleep apnea devices are able to provide the positive pressure needed for patients to maintain healthy oxygen levels, we still had to solve a few problems before these devices were fit for hospital use. First, we had to determine a way for patients to safely exhale while connected to their ventilator. Also, the air the patients inhale should have a level of moisture suitable for the lungs, while air exhaled should be as decontaminated as possible, for the safety of others. Finally, because the level of oxygen in the air was deemed insufficient, we decided the inlet of the CPAP/BiPAP machine should be infused with tank oxygen, as it's readily available in most hospital rooms.
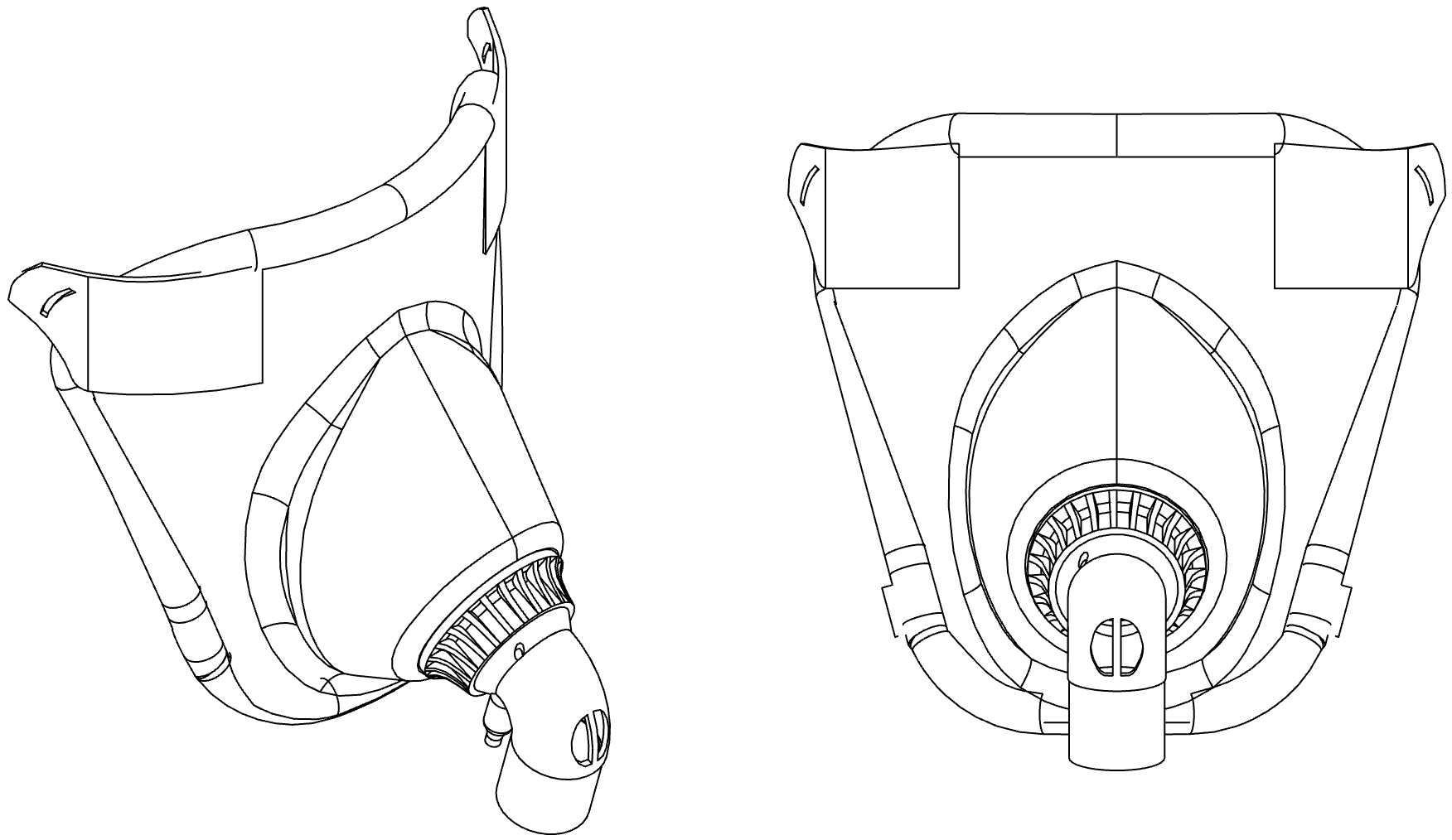
We solved the first of these issues by including an exhalation valve above the air hose. In order to both humidify and filter inhaled and exhaled air respectively, we also included a Hygroscopic Condenser Humidifier (HCH) & Filter normally found in hospital ventilators. In order to provide a solution at scale, it was important to find and use as many preexisting components as possible, rather than make them ourselves.
As well a creating the CAD models, assemblies, technical drawings, and renderings of the parts that comprise our solution, I contributed to our team’s effort by designing, testing, and fabricating a coupling to mate the inlet of the CPAP/BiPAP machines to external oxygen supplies. This component would allow us to mechanically vary the concentration of oxygen entering the sleep apnea machine, and ultimately the patient's lungs.
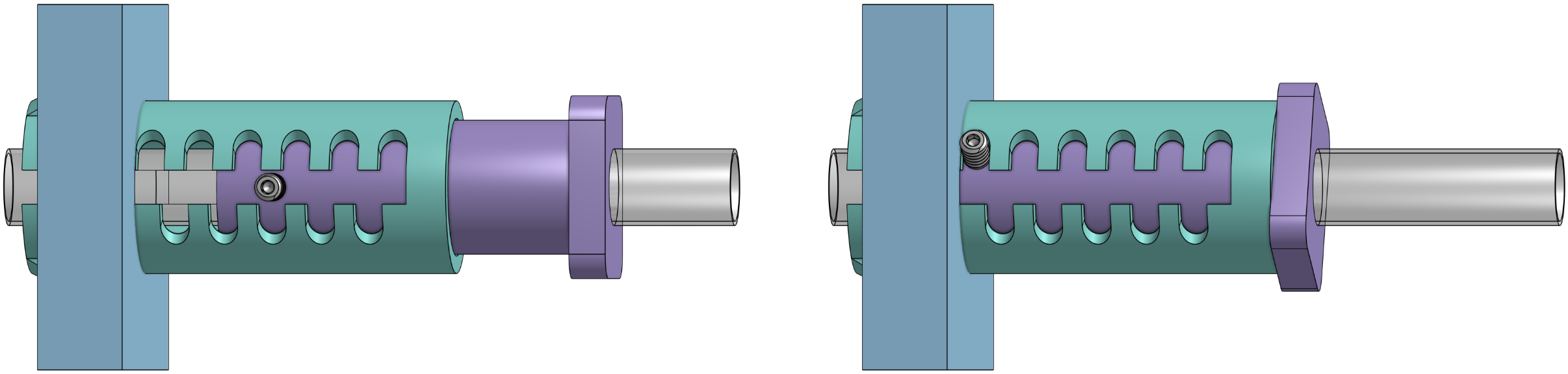
This design uses a piston (purple) and notched shell (teal) to form a sort of choking mechanism to restrict the amount of air that flows into the CPAP/BiPAP machine inlet (represented in blue).

After having designed, built, tested various prototypes, we were confident we had a solution that we could begin making into kits. These feature CPAP and BiPAP machines, as well as the remaining components necessary for medical professionals to assemble and operate functional ventilators, to begin to address the shortage faced by hundreds of hospitals across the US. Since then, group members have worked with non-profit businesses to handle the logistics of collecting sleep apnea machines from donors, as well as sourcing other parts from various medical supply companies. In the time since this project’s started, many hundreds of ventilator kits have been sent to hospitals not only in New York and California, but also to other countries in South America facing similar shortages.